“A very encouraging trend. Happy to see this change. Our emphasis on furthering all aspects relating to women empowerment remains very strong.”
-Prime Minister Narendra Modi
Maternal mortality has been an issue of concern in India for many years, and one of the country’s endless endeavours has been to improve maternal health and bring down the Maternal Mortality Ratio (MMR). MMR is the number of maternal deaths during a given time period per 100,000 live births during the same time period.[1] Maternal mortality in a region is a measure of the reproductive health of women in the area. Many women in reproductive age-span die due to complications during and following pregnancy and childbirth or abortion.

Maternal Mortality Ratio (MMR) in India was exceptionally high in 1990 with 556 women dying during child birth per hundred thousand live births. Approximately, 1.38 lakh women were dying every year on account of complications related to pregnancy and child birth.[2] The global MMR at the time was much lower at 385.
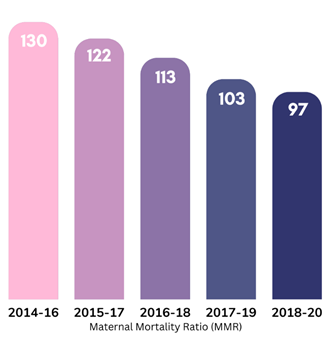
The National Health Policy (NHP) 2017 lay down the target to bring the MMR in India below 100/lakh live births by 2020. Owing to ceaseless efforts by the Government, India has successfully achieved the major milestone of bringing down its MMR to 97/lakh live births in 2018-20, well in time.[3]
The targeted interventions by the Government of India with the objective of addressing all aspects of maternal care have translated into a consistent decline in MMR over the last eight years. MMR in the country declined from 130 per lakh live births in 2014-16 to 122 in 2015-17, and further dropped by 9 points to 113 in 2016-18. By 2017-19, India’s MMR was already down to 103, against a global MMR of 211 (2017).
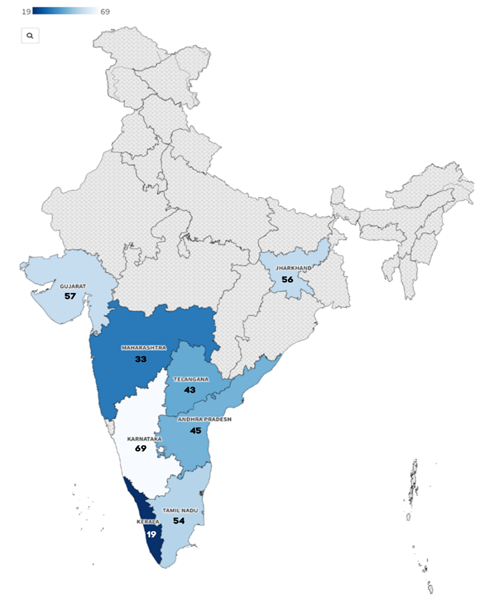
Target 3.1 in the Sustainable Development Goals (SDG) set by the United Nations in 2015 is to reduce the global MMR to less than 70/lakh live births by 2030. India is steadily advancing on the track to achieve this goal ahead of time with its policies for women’s health and wellbeing. The steps taken by the Central Government have facilitated outstanding progress by a number of states, eight of which have already achieved the SDG target. These include Kerala (19), Maharashtra (33), Telangana (43) Andhra Pradesh (45), Tamil Nadu (54), Jharkhand (56), Gujarat (57), and Karnataka (69).
|
The Government’s major focus area, in striving to bring down maternal mortality, has been to address the actual causes of mortality and morbidity among women, and deliver solutions to eliminate these causes. The emphasis has been on ensuring a continuum of care to address maternal and child health in a holistic manner, by providing excellent healthcare facilities to pregnant women, right from early stages of the pregnancy to postpartum care. Schemes have been designed keeping in mind the requirement of a range of medical facilities, right from testing and regular check-ups, to facilities for smooth delivery and further on to postnatal care of both mother and child.

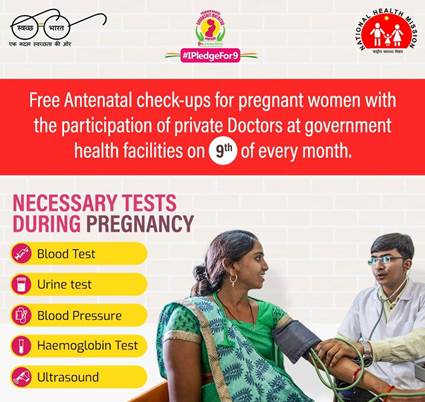
The efforts to boost maternal and new born care have given due attention to areas like antenatal care, nutrition for pregnant women and providing a positive birthing experience to mothers. Pradhan Mantri Surakshit Matritva Abhiyan, for instance, seeks to improve the quality and coverage of diagnostics and counselling services, along with providing assured comprehensive and quality antenatal care free of cost.[4]
Pregnant Women are among the major target groups of POSHAN Abhiyaan– the government’s flagship programme to improve nutritional outcomes. To further draw attention to the nutritional needs of this group, the Government of India’s focus for the 5th Rashtriya Poshan Maah (September 01 to 30, 2022) has been on maternal and child health. This year, the objective was to trigger Poshan Maah through Gram Panchayats as Poshan Panchayats with key focus on “Mahila aur Swasthya” and “Bacha aur Shiksha”.
To ensure a pregnancy without any financial woes, the Government has launched the Pradhan Mantri Matru Vandana Yojana (PMMVY), a direct benefit transfer (DBT) scheme under which cash benefits are provided to pregnant women in their bank account directly to meet enhanced nutritional needs and partially compensate for wage loss.
Providing a positive birthing experience to pregnant women has been made an imperative through programmes like Surakshit Matritva Anushasan (SUMAN), and Labour Room & Quality Improvement Initiative (LaQshya). SUMAN aims to provide assured, dignified and respectful delivery of quality healthcare services at no cost and zero tolerance of denial of services to any women and new born visiting a public health facility in order to end all preventable maternal and new born deaths and morbidities. This initiative has been built on the progress of schemes like Janani Shishu Suraksha Karyakram (JSSK) and Janani Suraksha Yojana (JSY).
LaQshya was launched with the objective of reducing maternal and new born mortality and morbidity, improving quality of care during delivery and immediate post-partum period, and enhancing positive birthing experience along with providing Respectful Maternity Care to all pregnant women attending public health facilities. The programme is working on improve quality of care for pregnant women in labour room, maternity Operation Theatre and Obstetrics Intensive Care Units (ICUs) & High Dependency Units (HDUs).[5]
These initiatives by the Government of India have played a pivotal role in increasing the number of institutional deliveries in the country. Institutional deliveries in India have increased substantially from 79 per cent in 2015-16 to 89 per cent in 2019-20. Around 87% births in rural areas and 94% births in urban areas are institutional deliveries. The government is also taking various other steps to promote institutional deliveries, like, operationalisation of Sub-Centres, Primary Health Centres, Community Health Centres and District Hospitals for providing 24×7 basic and comprehensive obstetric care, and capacity building of healthcare providers in basic and comprehensive obstetric care to enable them to provide high quality services during childbirth at the institutions.
Other initiatives include setting up of Maternal and Child Health (MCH) Wings at high caseload facilities to improve the quality of care provided to mothers and children, establishing Birth Waiting Homes (BWH) in remote and tribal areas to promote institutional delivery and improve access to healthcare facilities, and strengthening of over 25,000 ‘Delivery Points’ across the country in terms of infrastructure, equipment, and trained manpower. Comprehensive Abortion Care services are also being strengthened through trainings of health care providers, supply of drugs, equipment, Information Education and Communication (IEC) etc. The Union Ministry of Health and Family Welfare also launched the Anemia Mukt Bharat strategy in 2018 to reduce anaemia prevalence both due to nutritional and non-nutritional causes, in the lifecycle approach. The strategy is estimated to reach out to 450 million beneficiaries including 30 million pregnant women.
India’s achievement in bringing down MMR bolsters the Government’s resolve to ‘Surakshit Matritva Aashwasan’ for the women by creating a responsive health care system which strives to achieve zero preventable maternal and newborn deaths. As India celebrates its ‘Amrit Kaal’, the aim is to reduce MMR below the goal of 70/lakh live births, and maintain a steady decline going forward. To achieve this target, India is focusing on the standard of in-facility maternity care and raising awareness of the significance of reproductive health. The future that the Government of India envisions for the country is one where maternal mortality is no longer a cause for concern; with the various initiatives and healthcare facilities being introduced and diligently implemented, this vision is well on its way to becoming a reality.



